Naloxone (Narcan®) is a medication that can reverse the effects of an overdose from opioids, including fentanyl, heroin, and opioid-based pain killers. It is a tool that community members can use in emergency situations where opioid overdose occurs, providing a chance for individuals to receive further medical care and treatment.
Using Narcan
Used correctly, naloxone can reverse an opioid overdose. When Narcan is administered, it attaches to receptors in the brain and blocks opioids from having their usual effects. This helps to rapidly reverse an overdose by restoring normal breathing and providing an opportunity for medical assistance. There is no safety risk associated with naloxone.
How to Give Narcan
- Call 9-1-1
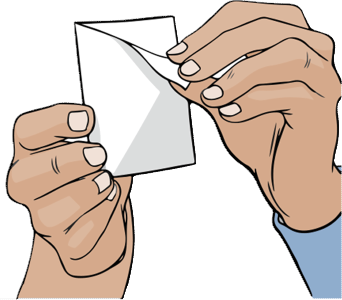
- Carefully remove Narcan from packaging
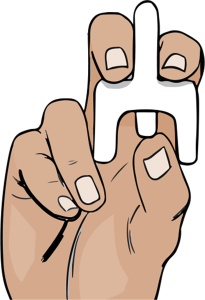
- Hold the nasal spray with your thumb on the plunger
- Tilt the individuals’ head back
- Place the tip of the nasal spray in either nostril of the person experiencing an overdose, firmly press the plunger and release the entire dose of medication.
- Wait 2-3 minutes while checking for responsiveness
- If there is no response, give additional dose, switching nostrils, until help arrives.




5-Step Guide for Giving Naloxone Nasal Spray(PDF, 389KB)
Remember to always dial 9-1-1 first.
Videos
Watch This 30-second Video for a Quick "Naloxone/Narcan How-To" (30 seconds):
The video below shows you the signs of an overdose and how to respond and take the steps to prevent opioid overdose.
For additional information on how to use Naloxone (Narcan®), dial 2-1-1 for information about where you can get trained on how to use Naloxone (Narcan®) in our community.
Carry a Narcan Kit With You
Opioid Overdose Prevention Programs (OOPPs) are organizations that provide individuals with training and a free Narcan kit to carry and dispense this potentially life-saving medication. OOPPs are registered by NYS Department of Health.
Free Narcan kits are available at one of the local registered OOPP community agencies listed below.
- TC Whole Health, 201 E. Green St., Ithaca (downtown), and 55 Brown Rd., Ithaca (northeast).
- Cayuga Addiction Recovery Services (CARS), 334 W. MLK/State St. Ithaca, 607-273-5500, ext. 5811.
- Cayuga Health Emergency Department, 101 Dates Dr., Ithaca
- REACH Medical, 1001 W. Seneca St., (First Floor), Ithaca
- Southern Tier AIDS Program (STAP), 314 W. MLK/State St., Ithaca. STAP also provides free Drug Checking services.
For additional options Dial 2-1-1 (1-877-211-8667) 24/7. Or text your Zip code to TXT211 (898211). Available M-F 9 AM to 4 PM
Pharmacy Standing Order
A statewide pharmacy standing order allows anyone to get naloxone (Narcan®) nasal spray at a pharmacy without a prescription in NYS. Ask for it at the pharmacy counter. Insurance covers up to $40 copay. If you don’t have insurance, you can buy naloxone at the pharmacy.
Note: Dispensing to adolescents under age 18 is at the discretion of the pharmacist.